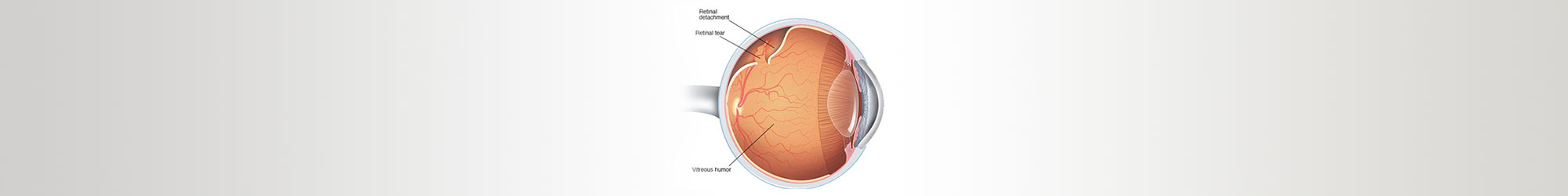
Retinal tear

The retina is a layer of specialized nerve tissue lining the back of the eye that allows you to see. The inside of the eye is filled with a gel-like substance called the vitreous. A retinal tear occurs when there is an abnormal attachment between the vitreous gel and the retina. In this case the vitreous gel can tug on the retina causing it to tear. Retinal tears can develop at any age, but tend to occur more commonly in the elderly. Tears are also more common in people who have myopiawho have a history of previous retinal tear or a family history of retinal tears or detachments. The flashing lights are typically much more noticeable at night or in the dark and can sometimes become more intense with eye movement. Floaters, on the other hand, are usually much more noticeable in strong light. Some people have a lot of these symptoms while others notice hardly anything at all.
Most retinal tears occur in the far peripheral retina, a part of the retina normally not used to see with. Therefore, most of the time there will be no noticeable change in the peripheral vision from the tear or the laser treatment. The laser treatment does not treat the floaters or flashing lights. These typically resolve gradually on their own over a period of weeks to months.
Laser treatment around the tear is the treatment of choice to heal the Retinal break.
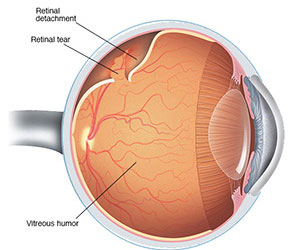
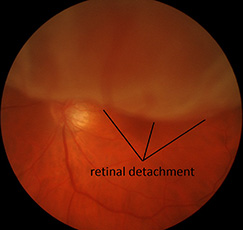
Retinal detachment
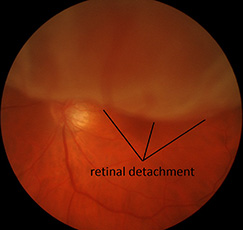
The retina is loosely attached to the back of the eye wall. When a retina detaches, it is lifted up from its normal position by fluid that accumulates between the retina and the eye wall. A detached retina is separated from its supply of oxygen and nutrition and does not work properly. Surgery is usually needed to reattach the retina to its normal position and prevent vision loss.
Retinal detachments can develop at any age, but tend to occur more commonly in the elderly. Retinal detachments usually occur around the time that the vitreous separates from the retina. This separation is a natural aging process in the eye and is called a posterior vitreous detachment (PVD). Most PVD’s cause no long-term damage to the eye, but in some individuals they result in retinal tears that can then lead to a retinal detachment.
Anyone who has an increased chance of developing a retinal hole or tear is at risk for developing a retinal detachment. Detachments are more likely to occur in people who are near-sighted (myopic), after an injury to the eye, after cataract surgery, or from weak areas in the retina. They are more common in people who have a history of previous retinal tear or a family history of retinal tears or detachments.
Peripheral retinal degeneration
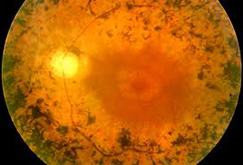
The far peripheral retina that is responsible for our extreme side vision can degenerate and become very thin and weak. The most common form of this peripheral retinal degeneration is lattice degeneration. Lattice degeneration is seen in about 1 out of every 10 people in the general population. When it occurs, it is common for the condition to be found in both eyes. Lattice degeneration also commonly leads to the development of retinal holes.
The cause is unknown but it is more common in people who are near-sighted (myopic) and tends to run in families.
Lattice degeneration can increase your risk of developing a retinal detachment. The retinal thinning, weakening and development of holes associated with lattice degeneration creates areas that are more prone to cause a retinal detachment. About one third of all retinal detachments are associated with lattice degeneration. Overall the lifetime risk of a retinal detachment in people with lattice degeneration is about 1 percent.
Usually there are no symptoms associated with Lattice Degeneration. Symptoms typically only occur when a complication from the lattice degeneration occurs, such as a tear or detachment of the retina. If you ever have the onset of flashing lights, new floaters or a loss of the side vision you need a prompt examination to rule out any serious problems with the retina.
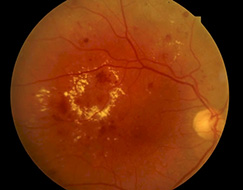
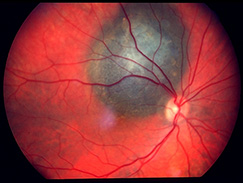
Age related macular degeneration (ARMD)
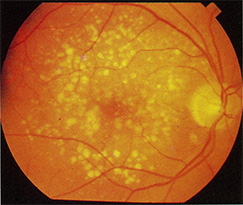
Age-related macular degeneration (ARMD) is a condition in which the macula is damaged as it ages, causing blurry and distorted vision. The condition affects both distance and close vision and can make some activities (like threading a needle or reading) very difficult or impossible. Macular degeneration is the leading cause of severe vision loss in people over 65.
The exact cause of macular degenerationis unknown. ARMD is clearly related to age and both genetic and environmental factors are important in the development of ARMD. From the genetic side, women, Caucasians, lightly-pigmented people (blond hair, fair skin, blue-eyed), and those with a strong family history have a higher chance of developing ARMD. From the environmental side, smoking, high blood pressure, high cholesterol, and obesity have been linked to the development and progression of ARMD.
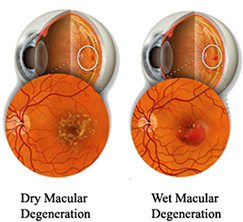
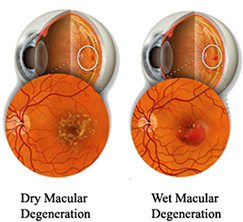
There are two types of AMD: wet and dry.
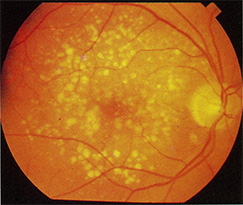
Dry ARMD: This is the most common form that accounts for 90% of cases of AMD. In dry ARMD tiny mounds of yellowish material called drusen collect under the retina. Over time the drusen can cause damage to the retina resulting in vision loss. This form of the disease is usually very slow, taking years or decades to cause varying degrees of visual symptoms, from minor to significant. Most people with dry ARMD retain good vision for their entire lives, although vision can be impaired in those with advanced dry ARMD.
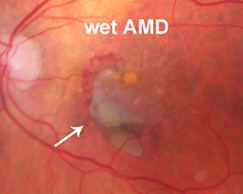
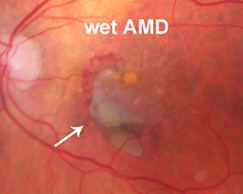
Wet ARMD: Wet ARMD always starts out as Dry ARMD, with a collection of drusen in the macula. If this progresses to wet ARMD, abnormal blood vessels begin to grow into the retina. The abnormal blood vessels are very fragile and can bleed and leak fluid, leading to vision losS. Although only about 10% of people ever develop Wet ARMD, it accounts for 90% of all of the severe vision loss from ARMD.
ARMD does not cause any pain. The symptoms of dry and wet ARMD can be different for different people. Often there are no symptoms at all, especially with dry ARMD. As the ARMD gets worse you may notice blurry vision, a dark or gray spot in the center of the vision, and distortion of the vision. Straight lines may appear wavy. As ARMD gets more severe, you may find it hard to read at all or to recognize faces at a distance. The symptoms of dry ARMD usually appear very slowly over many months or years. The symptoms of wet ARMD usually develop suddenly.
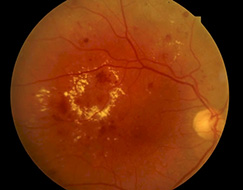
Diabetic retinopathy


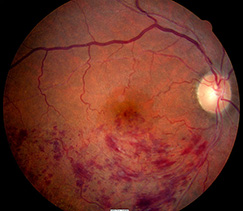
The abnormally high levels of blood sugar associated with diabetes can cause damage to the small blood vessels that supply oxygen and nutrients to the retina. Without the proper amount of oxygen and nutrients over time, the retina can become damaged. This damage to the retinal blood vessels is called diabetic retinopathy. The disease affects half of all people diagnosed with diabetes.
Diabetic retinopathy is classified as non-proliferative (NPDR) and proliferative diabetic retinopathy (PDR). There are various levels of severity of each kind of diabetic retinopathy and each is associated with different complications that can affect the vision. Mild diabetic damage to the retina may go unnoticed because early symptoms can be subtle, and tend to get worse over the years.
Anyone who has diabetes is at risk for retinopathy. Diabetic retinopathy is the most common cause of blindness in the 24-70 year age group. The risk of developing diabetic retinopathy increases the longer someone has the disease. Severe damage and vision loss are much more likely to develop if the diabetes is under poor control or has been under poor control in the past. For reasons not fully understood, pregnancy can accelerate the development of diabetic retinopathy as well.
Vision loss in diabetes is usually preventable with the appropriate treatment and care. The most important thing you can do to prevent vision loss from diabetes is to monitor and control your blood sugar and blood pressure. Ideally your Hemoglobin A1C should be maintained at 7.0 or less. Optimal control of blood sugar levels slows the onset and progression of diabetic retinopathy. Every diabetic should have a dilated eye examination at least once a year.
Hypertensive retinopathy

Due to high blood pressure, the retina’s blood vessel walls may thicken. This may cause your blood vessels to become narrow, which then restricts blood from reaching the retina. In some cases, the retina becomes swollen. Over time, high blood pressure can cause damage to the retina’s blood vessels, limit the retina’s function, and put pressure on the optic nerve, causing vision problems. This condition is called hypertensive retinopathy (HR).
Prolonged high blood pressure, or hypertension, is the main cause of HR. High blood pressure is a chronic problem in which the force of the blood against your arteries is too high. The force is a result of the blood pumping out of the heart and into the arteries as well as the force created as the heart rests between heartbeats. When the blood moves through the body at a higher pressure, the tissue that makes up the arteries will begin to stretch and will eventually become damaged. This leads to many problems over time.
The following conditions put you at a higher risk for HR: prolonged high blood pressure, heart disease, atherosclerosis, diabetes, smoking, high cholesterol, being overweight, eating an unhealthy diet and heavy alcohol consumption.
Additionally, the condition is more common in people of African descent, particularly Afro-Caribbean people. Women are also more likely to be affected by blood vessel damage than men.
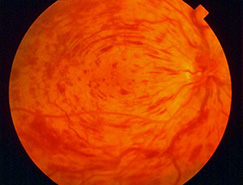
Retinal vein occlusion
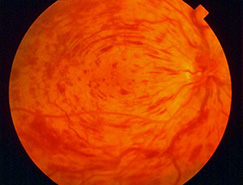
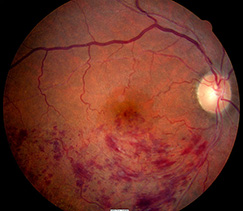
A retinal vein occlusion occurs when blood flow in one of the veins draining blood from the retina is reduced or blocked. Because blood that enters the eye cannot be drained properly through the blocked vein, the blood backs up in the retina creating areas of bleeding and swelling. The bleeding, swelling and lack of oxygen and nutrition in the retina can cause vision loss. Somewhat like a stroke occurring in the brain, in some cases the blockage in the vein can have very serious effects on the eye.
There are many different causes for a retinal vein occlusion. No single cause can explain the reason for every patient. The cause of a Retinal Vein Occlusion may be discovered thorough an evaluation of the retina or a general medical evaluation. Sometimes, the source of a Retinal Vein Occlusion cannot be identified, despite having a thorough examination and testing. Typically this condition occurs in individuals greater than 50 years old. Diseases that can contribute to the formation of a Retinal Vein Occlusion include high blood pressure, diabetes, heart disease, blood clotting disorders and glaucoma. The other eye can develop a retinal vein occlusion in 10% of people.
There are two major categories of retinal vein occlusions, branch and central retinal vein occlusions. The veinous drainage system for removing blood from the eye can be likened to a tree with many small branches draining into larger ones and ultimately into one central retinal vein (the tree trunk). In a branch retinal vein occlusion (BRVO) a small branch of the retinal venous system becomes blocked. In a central retinal vein occlusion (CRVO) the primary trunk of this vein can become blocked.
Retinal vein occlusions encompass a spectrum of disease ranging from mild, having little or no impact on the vision to severe, leading to blindness in the eye. The symptoms depend on the size and precise location of the blockage. Most patients note a sudden blurring or distortion of the vision that can be associated with a blind spot. The vision loss is usually not associated with any pain.
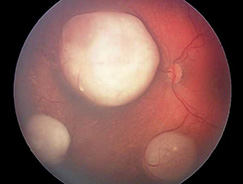
Retinoblastoma
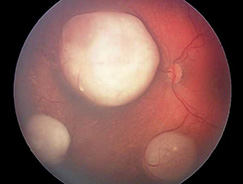
Retinoblastoma is a cancer that starts in the retina, the very back part of the eye. It is the most common type of eye cancer in children.
The eyes develop very early as babies grow in the womb. During the early stages of development, the eyes have cells called retinoblasts that divide into new cells and fill the retina. At a certain point, these cells stop dividing and develop into mature retinal cells. Rarely, something goes wrong with this process. Instead of maturing into special cells that detect light, some retinoblasts continue to divide and grow out of control, forming a cancer known as retinoblastoma. The chain of events inside cells that leads to retinoblastoma is complex, but it almost always starts with a change (mutation) in a gene called the retinoblastoma (RB1) gene. The normal RB1 gene helps keep cells from growing out of control, but the change in the gene stops it from working like it should.
If retinoblastoma tumors are not treated, they can grow and fill much of the eyeball. Cells might break away from the main tumor on the retina and float through the vitreous to reach other parts of the eye, where they can form more tumors. If these tumors block the channels that let fluid circulate within the eye, the pressure inside the eye can rise. This can cause glaucoma, which can lead to pain and loss of vision in the affected eye.
Choroidal melanoma
A melanoma is a type of cancer that results in the unregulated growth of the pigmented cells in the body called melanocytes. Melanomas can occur anywhere in the body where these pigmeted cells exist, including inside of the eye. Melanoma can occur in several areas of the eye including the iris, ciliary body, and choroids.
Choroidal melanomas are very rare, occurring in only about 6 people out of every million every year. Choroidal melanoma is the most common type of cancer to affect the eye in adults. The cause of melanoma is unknown. It most commonly occurs in mid-life and occurs equally in men and women. Caucasians are more likely to develop choroidal melanomas when compared to other groups. People with exposure to intense UV light (such as arc welders) have a slightly increased risk, but there are no other known environmental risk factors. Most commonly the melanoma grows from a pre-existing nevus (mole) in the eye.
The symptoms associated with a choroidal melanoma depends on where in the eye the melanoma beings to grow. In some cases there are no symptoms at all and the tumor is detected only on a routine examination. In some people a melanoma can cause blurred vision, flashing lights, floaters, or rarely pain.
Eale’s disease
Eales Disease is a rare disorder of sight that appears as an inflammation and white haze around the outercoat of the veins in the retina. The disorder is most prevalent among young males and normally affects both eyes. Usually, vision is suddenly blurred because the clear jelly that fills the eyeball behind the lens of the eye seeps out (vitreous hemorrhage).
Eales Disease usually presents as blurred vision resulting from oozing of the clear jelly-like substance from behind the lens of the eye. At the onset of the disorder, the small outer veins of the retina show sheathing (encapsulation or covering). As the disease progresses, the inflammation around the veins in the retina extends further behind the lens. Eales Disease may also be associated with peripheral retinal neovascularization which is the formation of new blood vessels on the outer part of the retina.
The more advanced cases of Eales Disease are characterized by a non- inflammatory degenerative disease of the retina (retinopathy) and extensive bleeding in the retina. The colorless jelly that fills the eyeball behind the lens oozes from the retina (vitreous hemorrhage) and, in rare cases, the retina may become detached. A reddish discoloration of the iris may be present (rubeosisiridis), and there may be loss of vision and damage to the optic disk (neovascular glaucoma). Clouding of the lens of the eye that obstructs the passage of light (cataracts) may develop as the disease progresses.
The exact case of Eales Disease is not known. This disorder seems to occur spontaneously because no precipitating factors such as injury, infection, or heredity appear to be involved.
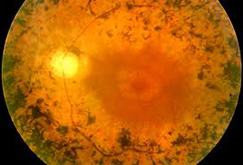
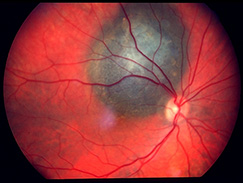
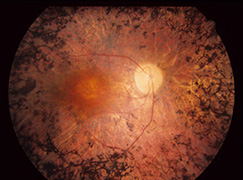
Retinitis pigmentosa
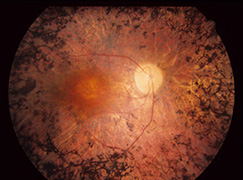
Retinitis pigmentosa (RP) is the name given to a group of inherited diseases where there is a genetic defect in the body that causes the retina to slowly stop working.
The most characteristic symptom is difficulty with night vision, and loss of side vision. Certain patients may have more problems with central vision and difficulty with bright lights. Difficulty with night vision is termed night blindness, often severely limiting function in the dark. As the disease progresses the side or peripheral vision continues to get worse. In the advanced stages of the disease only a small central island of vision may remain, termed tunnel. It is rare for patients to lose all vision in both eyes.
Most people with RP inherit the gene mutations from one or both of their parents. A mutated gene causes the nerve cells in the retina to function abnormally. There are currently over 100 different identified genetic defects in many different genes that can cause retinitis pigmentosa. The genetic mutations are usually passed on in one of three different patterns: autosomal dominant, autosomal recessive or X-linked. In autosomal dominant disease typically one parent has RP and passes the disease to 50% of their children. In autosomal recessive disease, neither parent has RP but both have abnormal genes. In this case 25% of their kids will get two bad copies and have RP. Lastly in X-linked RP the mother carries the mutation and usually does not have RP. 50% of her sons will have RP and none of her daughters will be affected.
Retinitis Pigmentosa is diagnosed based on a clinical examination and often confirmed with more advanced testing. Your ophthalmologist can diagnose retinitis pigmentosa by dilating the pupils and examining the retina. Often there are clumps of pigment noted at the back of the eye (figure 1). Further testing with formal visual field test can be done to tell how much peripheral vision is remaining. A special test called an electroretinogram (ERG) can test the electrical function of the retina. In some cases the exact genetic defect can be identified through genetic testing. The tests are more likely to give a meaningful answer if a number of affected family members can all be tested at the same time.